Ask the Flight Surgeon / By MAJ (Dr.) Joseph R. Adams: Q: I’ve begun to experience a pins-and-needles sensation in my hand while flying and for some time after shutdown. Should I be concerned?
Q: I’ve begun to experience a pins-and-needles sensation in my hand while flying and for some time after shutdown. Should I be concerned?
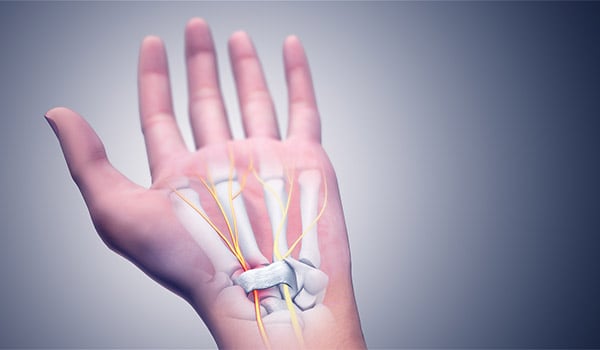
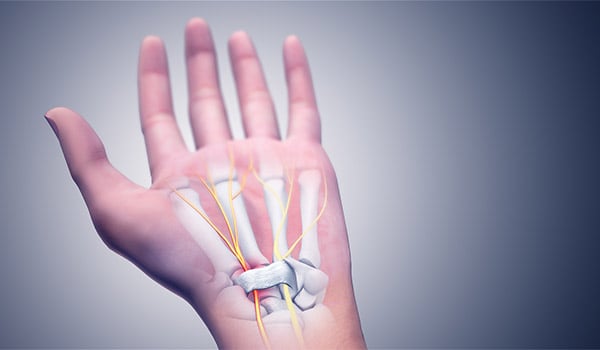
Carpal Tunnel Syndrome / WIKIMEDIA COMMONS GRAPHIC
FS: The medical terminology for numbness and tingling is paresthesia. Paresthesia of the hand is a common complaint among aviators, and especially among rotary-wing pilots. Symptoms of paresthesia can include numbness, tingling, itching, prickling, pins-and-needles sensation, and pain. While these symptoms may not be harmful and can be self-limited, there are a number of causes that can lead to permanent deficits and flight conditions that are potentially dangerous. Of particular concern to aviators are the potential for impairment of fine motor coordination, loss of strength, and changes or complete loss of sensation in the fingers and hands that are critical for safety of flight. Always inform your Flight Surgeon if you experience any paresthesia.
Causes
There are several potential causes, from nerves to blood vessels to certain disorders. Nerves can be affected anywhere along their path from the brain to the hand. Compressed nerves can be a cause and can result from your body position while flying or from entrapment of the nerves in the elbow, between vertebrae in the neck, or within compartments of the wrist such as in carpal tunnel syndrome. Restricted blood-flow to the hand due to tight clothing or equipment is also a potential culprit. Other possible reasons for paresthesia include autoimmune disease, endocrine disease, toxicity, and infection.
The most important consideration in determining the cause of paresthesia is the history, or background information, that you provide to your Flight Surgeon. Some important considerations are:
- How long have you been experiencing symptoms?
- Was there an injury or other trauma?
- What triggers the symptoms?
- Are the symptoms constant or intermittent?
- If intermittent, how long do they last?
- What makes your symptoms worse (certain positions, certain clothing, vibrations, certain medications, etc.)?
- What makes them better?
- How are your symptoms distributed (specific fingers, one hand, both hands, hands and feet, etc.)?
- Are there any other associated symptoms (weakness, numbness, loss of coordination, discoloration, cold sensation, neck pain)?
- If there is pain, does it radiate up your arm or does it stay in one place?
- Are you taking any medications?
- What do you do in your free time? (potential tick exposures, high-risk sexual activities, etc.)
- Do you have any medical conditions (diabetes, gastrointestinal disease, scoliosis, autoimmune disease, etc.)?
- Is there a family history of illness such as diabetes, Raynaud’s, muscular dystrophy, or anything else?
The approach to diagnosing the cause of paresthesia depends largely on the answers to the questions above in relation to the symptoms. In some cases, the cause will be obvious based on the history. In many cases, however, it will be necessary to narrow down the list of potential causes by performing physical maneuver examinations or lab testing. The lab tests may include blood tests for thyroid function, presence of infections such as Lyme disease or Syphilis, vitamin levels, presence of heavy metals, and levels of inflammatory markers, among others. It may also be necessary to perform further nerve studies such as electromyography (EMG), nerve conduction velocities (NCV), and evoked potential tests. You may also be referred to a neurologist for further evaluation.
Treatment of paresthesia is entirely dependent on the underlying cause. Given the broad range of potential causes, it is crucial to first identify the exact cause. Once a diagnosis has been made, treatment may range from wearing a brace or discontinuation of a medication to the surgical decompression of an entrapped nerve or use of antibiotic medication.
Prognosis
Due to the potential for complications or progression of symptoms, grounding is frequently required until the cause of a paresthesia can be identified or until symptoms have resolved to conserve safety of flight. The good news is that the prognosis for recovery is very good once the correct treatment is provided. In some cases, it may be necessary to demonstrate full recovery through simulator evaluation, cockpit egress testing, or other functional testing prior to return to full flight duty.
Fly Safe!
Questions?
If you have a question you would like addressed, email it to This email address is being protected from spambots. You need JavaScript enabled to view it.; we’ll try to address it in the future. See your unit flight surgeon for your personal health issues. The views and opinions offered are those of the authors and researchers and should not be construed as an official Department of the Army position unless otherwise stated
MAJ (Dr.) Joseph R. Adams is a flight surgeon at the School of Army Aviation Medicine, Fort Rucker, AL.