Ask the Flight Surgeon / Dr. (LTC) Joseph Puska: Q: I was recently diagnosed with Atrial fibrillation and prescribed Coumadin (warfarin) and a calcium channel blocker (Diltiazem) for heart rate control. I saw a cardiologist who took me off the medications, and used radio-frequency ablation to eliminate the fibrillation, but I still have a high heart rate (118 to 126), don’t have my normal energy level, and I’m running much slower than usual. What’s the next step?
 FS: As in any medical condition, the first and most important thing is to take care of you by treating the condition, and worry about returning you to flight status after your heart rate is back to normal, and you hopefully don’t need to continue medication. In this case, since it’s been over two months since the ablation therapy, and that has been unsuccessful, we’ll refer you back to the cardiologist who has recently treated you, and is familiar with your case. If there is to be a significant delay in getting back to the cardiologist it would seem reasonable to re-start the medications you were taking before the procedure even though medical treatment is not compatible with flight status for the time being.
FS: As in any medical condition, the first and most important thing is to take care of you by treating the condition, and worry about returning you to flight status after your heart rate is back to normal, and you hopefully don’t need to continue medication. In this case, since it’s been over two months since the ablation therapy, and that has been unsuccessful, we’ll refer you back to the cardiologist who has recently treated you, and is familiar with your case. If there is to be a significant delay in getting back to the cardiologist it would seem reasonable to re-start the medications you were taking before the procedure even though medical treatment is not compatible with flight status for the time being.
Physiology
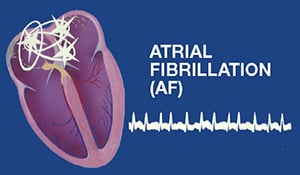
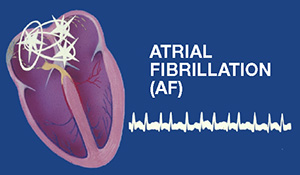
In a normally beating heart, an electrical impulse is generated near the top of the right atrium in the sino-atrial (SA) node that then travels at a steady rate though the atria causing them to contract, and then through the atrio-ventricular node at the junction between the atria of the upper heart and the main pumping chambers the ventricles, causing them to contract forcefully in a nicely synchronized fashion just after the atria that fill them do. In atrial fibrillation (A-fib), impulses are randomly generated in locations other than the SA node (usually the ends of the pulmonary veins near the heart) that cause the atria to contract very irregularly or fibrillate. This can be asymptomatic, but can cause some people to notice heart fluttering or palpitations, and some fatigue and weakness as in your case. The “atrial kick” provides roughly 5% of cardiac output, but in trained athletes it can be closer to 15%. Blood lying against the walls of the atria for prolonged periods can form a clot called a mural thrombus. Pieces of the clot can break free causing pulmonary emboli or a stroke. The Coumadin was given to you to prevent the clot from forming, and the calcium channel blocker to slow the heart rate down; other medications can be used to try to put the heart back into a regular rhythm.
Risks and Treatment
Radio-frequency ablation is done by inserting very thin wires inside the heart through a large vein, finding the tiny areas that are causing the atria to beat irregularly, and then destroying those tissues with high heat. It is successful approximately 74% of the time.
Atrial fibrillation is the most common cardiac arrhythmia. For every decade of life the prevalence doubles, and by the age of 80-90, 10% of people have it. The most common cause is hypertension, and other risk factors include hyperthyroidism, chronic obstructive pulmonary disease, pneumonia, pulmonary embolism, rheumatic heart disease, mitral stenosis, structural heart disease, and pericardial disease. Obesity, heavy alcohol use (“holiday heart”), and metabolic syndrome also contribute to the risk. Smoking and heavy caffeine intake can also be contributing. Men are more likely to develop atrial fibrillation, but it is more dangerous in terms of outcome for women. All of these possible causes should be sought out by the health care team, and any reversible ones identified and treated.
Workup should include a metabolic panel, thyroid panel, echocardiography, and invasive or non-invasive testing for cardiac ischemia based upon calculated likelihood, and a cardiology consult. Also required for waiver submission are an AGXT, and three 24-hour Holter monitor studies done at two-month intervals. A detailed health history to document any precipitating event, and a six-month observation period off of anti-arrhythmic or rate controlling medications without recurrence is necessary for waiver.
Flying Duty
A single episode of atrial fibrillation with clearly documented precipitating factors (e.g. “holiday heart”) is waiverable for flying duty following a six month period of observation to ensure absence of recurrence as well as the elimination of underlying organic sources. In your case, a waiver may be applied for six months after successful radio frequency ablation, with a normal post-ablation evaluation (A fib unable to be provoked) on a case-by-case basis. Hopefully the second attempt will be effective. Waivers are not recommended for recurrent cases, or cases with significant underlying coronary artery disease. Initial applicants with a history of A-fib are not considered for exception to policy. Safe flying, and see you at the flight line! —Doc Puskar
Question for the Flight Surgeon?
If you have a question you would like addressed, email it to This email address is being protected from spambots. You need JavaScript enabled to view it.; we’ll try to address it in the future. See your unit flight surgeon for your personal health issues. The views and opinions offered are those of the author and researchers and should not be construed as an official Department of the Army position unless otherwise stated
Dr. (LTC) Joseph Puskar is a flight surgeon and the director of the Army Flight Surgeon Primary Course at the US Army School of Aviation Medicine at Fort Rucker, AL